Malaria is a life-threatening infectious disease caused by Plasmodium parasites. These parasites are transmitted to humans through the bites of infected female Anopheles mosquitoes. Malaria remains a significant public health concern, particularly in tropical and subtropical regions where the Anopheles mosquito thrives.

Causes and Transmission
Malaria is caused by Plasmodium parasites, which are transmitted to humans through the bites of infected female Anopheles mosquitoes. Here’s a breakdown of how the disease is caused:
- Parasite Transmission: Malaria parasites belong to the genus Plasmodium. Several species of Plasmodium can cause malaria in humans, including Plasmodium falciparum, Plasmodium vivax, Plasmodium ovale, Plasmodium malariae, and Plasmodium knowlesi. When an infected female Anopheles mosquito bites a person to feed on blood, it injects saliva containing the malaria parasites into the bloodstream of the human host.
- Liver Stage: Once inside the human body, the malaria parasites travel to the liver, where they undergo a phase of maturation and replication known as the liver stage. During this stage, the parasites multiply inside hepatocytes (liver cells) without causing symptoms.
- Blood Stage: After the liver stage, the parasites re-enter the bloodstream and infect red blood cells, initiating the blood stage of infection. Inside the red blood cells, the parasites continue to multiply rapidly, leading to the destruction of the infected cells. This cycle of invasion, replication, and destruction of red blood cells is responsible for the characteristic symptoms of malaria, such as fever and chills.
- Transmission to Mosquitoes: When an infected person is bitten by another female Anopheles mosquito, the mosquito ingests the malaria parasites along with the person’s blood. Inside the mosquito’s body, the parasites undergo further development and maturation, eventually reaching the stage where they can infect another human host during a subsequent blood meal.
- Cycle Continuation: The transmission cycle continues as infected mosquitoes bite new human hosts, perpetuating the spread of malaria in endemic area.
Types
Malaria is caused by several species of Plasmodium parasites, and each species can result in different types or forms of the disease. The most common types of malaria include:

- Plasmodium falciparum malaria: This is the most severe and potentially life-threatening form of malaria. Plasmodium falciparum is responsible for the majority of malaria-related deaths worldwide. It can lead to complications such as cerebral malaria, severe anemia, organ failure, and death if not promptly treated. Falciparum malaria is prevalent in sub-Saharan Africa but can also be found in other regions with suitable environmental conditions.
- Plasmodium vivax malaria: Plasmodium vivax is the second most common species of malaria parasite and is widespread in Asia, Latin America, and parts of Africa. While it’s generally less severe than falciparum malaria, it can still cause significant illness. Vivax malaria can lead to relapses because the parasite can form dormant stages in the liver known as hypnozoites, which can reawaken and cause recurrent infections months or even years after the initial infection.
- Plasmodium malariae malaria: This type of malaria is caused by Plasmodium malariae and is generally less severe than falciparum malaria. It tends to cause chronic, low-grade infections that can persist for many years if left untreated. Malariae malaria is found in tropical and subtropical regions worldwide.
- Plasmodium ovale malaria: Plasmodium ovale is similar to P. vivax in that it can form dormant liver stages (hypnozoites), leading to relapses. It is less common than other species of malaria and is primarily found in West Africa, although cases have been reported in other regions.
- Plasmodium knowlesi malaria: Plasmodium knowlesi is a malaria parasite that primarily infects monkeys but can also infect humans. In recent years, human infections with P. knowlesi have become increasingly recognized, particularly in Southeast Asia. It can cause severe disease in humans and is sometimes misdiagnosed as other forms of malaria.
Each type of malaria can present with similar symptoms, including fever, chills, headache, muscle aches, fatigue, and nausea. However, the severity of the disease and the risk of complications can vary depending on the species of Plasmodium involved, as well as factors such as the individual’s immune status and access to healthcare. Proper diagnosis and prompt treatment are essential for effectively managing malaria and preventing complications.
Symptomes
The symptoms of malaria can vary depending on factors such as the species of Plasmodium parasite causing the infection, the individual’s immune status, and whether they have received any prior treatment for malaria. However, common symptoms of malaria typically include
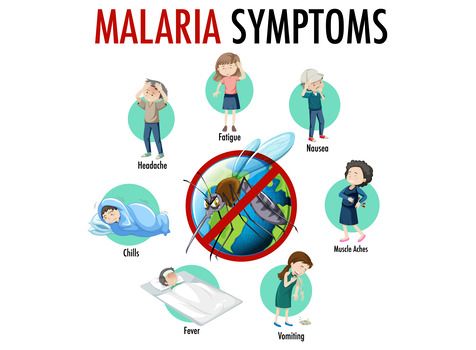
- Fever: Fever is one of the hallmark symptoms of malaria. It may be intermittent (coming and going) or continuous, and the severity can vary. The fever may be accompanied by chills and rigors, especially during the onset of fever episodes.
- Chills: Chills often accompany fever episodes in malaria. They may be intense and uncontrollable, leading to shaking and shivering.
- Headache: Headaches are common in malaria and can range from mild to severe. They may be generalized or localized to specific areas of the head.
- Muscle and Joint Pain: Malaria infection can cause muscle aches and joint pain, which can be widespread or localized.
- Fatigue: Many individuals with malaria experience fatigue, weakness, and a general feeling of malaise.
- Nausea and Vomiting: Some people with malaria may experience nausea and vomiting, which can contribute to dehydration and further weakness.
- Sweating: Profuse sweating often occurs as the fever breaks during the course of the illness, particularly in cases of intermittent fever.
- Anemia: Malaria can lead to the destruction of red blood cells, resulting in anemia. Symptoms of anemia may include weakness, paleness, and shortness of breath.
- Enlarged Spleen and Liver: In some cases, malaria can cause enlargement of the spleen and liver, which may be palpable upon physical examination.
- Cognitive Symptoms: In severe cases, particularly with cerebral malaria caused by Plasmodium falciparum, individuals may experience confusion, altered consciousness, seizures, and coma.
Prevention
Prevention of malaria involves a combination of strategies aimed at reducing the risk of mosquito bites and preventing the transmission of the malaria parasite. Here are some key methods for preventing malaria.
Vector Control:
- Insecticide-Treated Bed Nets (ITNs): Sleeping under insecticide-treated bed nets can significantly reduce the risk of mosquito bites, especially during the night when Anopheles mosquitoes, the vectors of malaria, are most active.
- .Indoor Residual Spraying (IRS): IRS involves applying insecticides to the interior walls of houses and other structures to kill mosquitoes that come into contact with the treated surfaces. This method can help reduce mosquito populations indoors.
Personal Protection Measures:
- Use of Repellents: Applying mosquito repellents containing DEET (N,N-diethyl-meta-toluamide), picaridin, or other recommended active ingredients to exposed skin can help repel mosquitoes.
- Wearing Protective Clothing: Wearing long-sleeved shirts, long pants, socks, and closed-toe shoes can help reduce exposure to mosquito bites, especially during outdoor activities in malaria-endemic areas.
Chemoprophylaxis (Preventive Medication):
- For individuals traveling to malaria-endemic regions, especially areas with chloroquine-resistant Plasmodium falciparum, taking prophylactic antimalarial medication as prescribed by a healthcare provider is recommended. Common antimalarial drugs for chemoprophylaxis include atovaquone-proguanil, doxycycline, and mefloquine.
- It’s important to start preventive medication before traveling to a malaria-endemic area, continue taking it during the trip, and adhere to the prescribed dosage regimen. Some medications need to be started before travel, while others can be started upon arrival in the malaria-endemic area.
Environmental Management:
- Reducing Mosquito Breeding Sites: Efforts to eliminate or reduce standing water, where mosquitoes breed, can help reduce mosquito populations. This includes draining stagnant water from containers, covering water storage containers, and improving drainage systems.
- Environmental Modifications: Modifying the environment to minimize human-mosquito contact, such as clearing vegetation around homes and using screens on windows and doors, can help reduce indoor mosquito entry.
Community-Based Interventions:
- Community engagement and education programs can raise awareness about malaria prevention methods, promote the use of preventive measures, and encourage early diagnosis and treatment of malaria cases within communities.
- Integrated vector management (IVM) approaches, which combine multiple interventions tailored to local settings, can be effective in controlling malaria transmission.
Diagnosis
Diagnosis of malaria typically involves a combination of clinical evaluation and laboratory testing. Here are the common methods used for diagnosing malaria:
- Clinical Assessment: Healthcare providers begin by evaluating the patient’s symptoms and medical history, including recent travel to malaria-endemic areas. While clinical symptoms such as fever, chills, and headache can raise suspicion of malaria, they are not specific to the disease and can overlap with other febrile illnesses. Therefore, a definitive diagnosis requires laboratory confirmation.
- Microscopic Examination of Blood Smears: Microscopic examination of blood smears remains the gold standard for malaria diagnosis. A small drop of blood obtained from a finger prick or venous blood is placed on a microscope slide, stained with a special dye (e.g., Giemsa stain), and examined under a microscope to detect the presence of malaria parasites within red blood cells. This method allows for the identification of the malaria parasite species and determination of parasite density, which can help guide treatment decisions.
- Rapid Diagnostic Tests (RDTs): Rapid diagnostic tests are simple, easy-to-use diagnostic tools that detect specific malaria antigens in a patient’s blood sample. RDTs provide rapid results within 15 to 20 minutes and do not require specialized laboratory equipment or skilled personnel, making them particularly useful in resource-limited settings where microscopy may not be readily available. However, RDTs may have limitations in terms of sensitivity and specificity, especially in detecting low levels of parasitemia or differentiating between species.
- Molecular Tests: Polymerase chain reaction (PCR) and other molecular techniques can detect and identify malaria parasites’ genetic material (DNA or RNA) with high sensitivity and specificity. These tests are particularly valuable for confirming malaria diagnosis in cases where microscopy and RDT results are inconclusive or when differentiating between species is necessary. However, molecular tests are more complex, expensive, and require specialized laboratory facilities and trained personnel, limiting their availability in some settings.
- Other Diagnostic Methods: In some cases, additional laboratory tests may be used to evaluate complications of malaria or assess the patient’s overall condition, such as complete blood count (CBC) to detect anemia or liver function tests to assess liver damage.
Treatment
The treatment of malaria depends on several factors, including the species of Plasmodium parasite causing the infection, the severity of the illness, the patient’s age, pregnancy status, and any underlying health conditions. Prompt and effective treatment is crucial to prevent complications and reduce mortality associated with malaria. Here are the main components of malaria treatment:
- Antimalarial Medications: Antimalarial drugs are used to kill the malaria parasites and cure the infection. The choice of antimalarial medication depends on factors such as the species of Plasmodium parasite and the drug resistance patterns in the region where the infection was acquired. Some commonly used antimalarial medications include:
- Artemisinin-based Combination Therapies (ACTs): ACTs are the recommended first-line treatment for uncomplicated falciparum malaria, the most severe form of malaria. These combinations typically contain an artemisinin derivative (e.g., artemether or artesunate) combined with another antimalarial drug (e.g., lumefantrine, piperaquine, or mefloquine). ACTs are highly effective and rapidly reduce the parasite burden.
- Chloroquine: Chloroquine was once widely used for treating malaria caused by Plasmodium vivax, Plasmodium ovale, and some strains of Plasmodium malariae. However, resistance to chloroquine has become widespread in many regions, limiting its effectiveness.
- Quinine and Quinidine: Quinine and its derivative quinidine are still used in some regions for treating severe malaria, particularly when artemisinin-based therapies are not available or contraindicated. Quinine is often combined with an antibiotic such as doxycycline or clindamycin for greater efficacy.
- Other Antimalarials: In addition to the above medications, other antimalarial drugs such as atovaquone-proguanil (Malarone), primaquine, and tafenoquine may be used for specific purposes, such as preventing relapse in vivax or ovale malaria or clearing liver-stage parasites.
- Supportive Care: In severe cases of malaria or when complications arise, supportive care may be necessary to manage symptoms and prevent organ damage. Supportive measures may include intravenous fluids to maintain hydration, blood transfusions for severe anemia, antipyretic medications to reduce fever, and treatment of complications such as respiratory distress or renal failure.
- Follow-up Monitoring: After initiating treatment, patients with malaria should be closely monitored for clinical improvement and resolution of symptoms. In some cases, follow-up blood tests may be performed to confirm parasite clearance and ensure treatment success.
- Prevention of Recurrence: In regions where Plasmodium vivax or Plasmodium ovale are prevalent, additional treatment with primaquine or tafenoquine may be necessary to prevent relapse by targeting dormant liver-stage parasites (hypnozoites).
HOMEOPATHY
In homeopathy, remedies are selected based on the principle of “like cures like” and the individualized presentation of symptoms. While there are homeopathic remedies that practitioners might consider for supporting the body during and after a malaria infection, it’s crucial to emphasize that homeopathy is not a replacement for conventional medical treatment for malaria. Malaria can be a severe and potentially life-threatening disease, and prompt, effective treatment with antimalarial drugs is essential.
That said, some homeopathic remedies might be considered for managing symptoms associated with malaria or supporting the body’s recovery. However, these remedies should only be used as adjunctive or complementary treatments under the supervision of a qualified healthcare professional, and they should not delay or replace conventional medical care. Additionally, individualized constitutional treatment, based on the totality of symptoms and the patient’s overall health, is a fundamental principle of homeopathy.
Some homeopathic remedies that might be considered for managing symptoms associated with malaria include:
- China Officinalis (China or Cinchona): This remedy is often indicated for debility, weakness, and exhaustion following loss of vital fluids (such as sweating, vomiting, or diarrhea), which can occur in malaria. It may also be considered for periodic fevers with chills and shaking.
- Arsenicum Album: Arsenicum is indicated for individuals experiencing restlessness, anxiety, burning pains, and weakness, which are common symptoms in malaria. It may also be considered for diarrhea or vomiting associated with the illness.
- Natrum Muriaticum: Natrum mur is indicated for individuals who experience periodic fevers with chilliness, particularly if there is a history of suppressed emotions or grief. It may also be considered for headaches and weakness associated with malaria.
- Gelsemium: Gelsemium is indicated for individuals who experience weakness, lethargy, and heaviness, particularly when there is a sensation of trembling or trembling during the fever. It may also be considered for headaches and muscle aches.
- Eupatorium Perfoliatum: Eupatorium is indicated for intense bone pains, especially in the back and limbs, which are common symptoms in malaria. It may also be considered for fever with great thirst.
Complication
Malaria, if left untreated or if treatment is delayed, can lead to various complications, some of which can be severe and life-threatening. These complications can affect different organs and systems in the body. Here are some common complications associated with malaria:
- Severe Anemia: Malaria can cause the destruction of red blood cells, leading to anemia. Severe anemia can result in fatigue, weakness, shortness of breath, and in severe cases, organ failure.
- Cerebral Malaria: This is a severe form of malaria caused by Plasmodium falciparum and is characterized by the involvement of the brain. Cerebral malaria can lead to neurological symptoms such as confusion, altered consciousness, seizures, coma, and even death if not promptly treated.
- Multi-organ Dysfunction: Severe malaria can lead to dysfunction of multiple organs, including the kidneys, liver, and lungs. This can result in complications such as acute kidney injury, liver failure, pulmonary edema (fluid accumulation in the lungs), and acute respiratory distress syndrome (ARDS).
- Hypoglycemia: Malaria, especially in children and pregnant women, can cause low blood sugar levels (hypoglycemia), which can lead to weakness, seizures, loss of consciousness, and coma if not managed promptly.
- Pregnancy Complications: Pregnant women are at increased risk of severe malaria and its complications. Malaria during pregnancy can lead to miscarriage, stillbirth, preterm delivery, low birth weight, and maternal mortality.
- Metabolic Acidosis: Severe malaria can disrupt the body’s acid-base balance, leading to metabolic acidosis, which is characterized by an accumulation of acid in the blood. Metabolic acidosis can impair organ function and contribute to the severity of malaria.
- Hyperparasitemia: In some cases of severe malaria, there is a high level of parasitemia (parasites in the bloodstream), known as hyperparasitemia. This can increase the risk of complications such as organ failure and death.
- Long-term Neurological Sequelae: Survivors of cerebral malaria may experience long-term neurological sequelae, including cognitive impairment, motor deficits, behavioral changes, and epilepsy.